Never Forsaken
July 31, 2020The two main types of transplantation used to treat non-Hodgkin lymphoma are autologous and allogeneic. Allogeneic stem cell transplantation uses stem cells from a donor, usually a close blood relative or someone who is a genetic match with similar blood and tissue types. The goal is the same as with an autologous transplant: to repopulate the bone marrow with stem cells. These cells then develop into healthy white blood cells that can mount an immune response that destroys non-Hodgkin lymphoma cells in your body. But it carries more risk than autologous transplant: the donor stem cells may see your healthy cells as foreign, attacking them in a condition called graft-versus-host disease, or your body may see the donor stem cells as foreign, creating an unhealthy immune response. (Perlmutter Cancer Center, NYU Langone)
Basically, I needed my sister’s stem cells to fight my cancer cells or whatever remains of it. Through this, we hoped I will remain in remission for a long time. My stem cell transplantation (SCT) journey began on May 9, with my sister as my initial caregiver. I was admitted to the hospital and was inserted with a central line in my femoral vein.
For the next 5 days, I had chemotherapy, cyclophosphamide and fludarabine, which I tolerated well.
On May 15, I went through total body irradiation (TBI). The experience was peculiar; I had to be naked! Gratefully, the staff was nothing short of professional. The procedure itself was short, around fifteen minutes on each side of the body. But the preparation took long. I lay in the table, and there were lots of hands strapping, positioning, measuring, and putting electrodes on me. They also covered me in water bags! That, I didn’t know what for.
I needed the chemotherapy and TBI to suppress my immune system prior to transplant. Hence, after the TBI, I was transferred from a regular room to the SCT unit, where there was strict isolation precautions. My mother came with me in the unit as my caregiver. Meanwhile, few doors down, my sister got admitted as the donor.
On May 16 and 17, I had my rebirthday. I was reborn with a new immune system. I was given another fighting chance in life. It was Day 0.
My sister had her stem cells harvested through a femoral vein access and using an apheresis machine in 4 hours. The stem cells were then immediately transfused to me. We had to do it twice because on the 16th, we only had 2.5 million stem cells, and I needed 5 million stem cells. God multiplied what we lacked! On the 17th, we had 4.7 million stem cells. My sister was then able to go home on the 18th.
I knew that the days following a transplant will be tough but I didn’t expect how terrible they were! Right after my second infusion of stem cells, I began having some reactions. My eyes were swollen and I started having fever. My oncologist also told us that on Day 3 and Day 4, I will receive high-dose cyclophosphamide. My blood counts are expected to drop, so I have to prepare at least four blood donors for red blood cell and platelet transfusions.
The following two weeks in the SCT unit, I was a wreck.
On the first week, my fever continued, and I had pulmonary congestion. I needed oxygen support. I was started on antibiotics and diuretics. I was inserted with a Foley catheter to drain and measure my urine. However, we had to change the catheter size thrice because of a leak. We eventually had to remove it, but my urethra was already irritated. My hemorrhoids also started acting up. Thus, the pain I experienced during urination and bowel movement was unimaginable!
Blood transfusions were also started. With the current pandemic, it was more difficult to acquire blood products. Thank God, we were able to get help. Because my blood pressure was dropping, dopamine drip was started too. Moreover, I went through a KUB (kidney, ureter, and bladder) ultrasound and an echocardiogram to check my abdomen and chest because I was having pains in these areas. A lot was happening in the first week!
On the second week, I was restless. I wanted to be out of the SCT unit, but my white blood cells (WBCs) were still nonexistent. We were waiting for the stem cells to engraft and produce a minimum amount of WBCs before I can be transferred to a regular room.
Meanwhile, I was dealing with an awful edema, the accumulation of fluid. When my blood counts started to drop, specifically my platelet, I had to stop my anticoagulant. When my intestines were inflamed, I had to stop consuming food and water for 48 hours, and I was given total parenteral nutrition, food directly to my veins. Both of these while I still had other intravenous infusions and while my mobility was already very limited. No wonder my body’s circulation was messed up. My admission weight was 47 kg, but I weighed 54 kg—that’s 7 kg of fluid accumulation. I was so swollen. I felt like exploding!
I cried so hard to God. I kept questioning Him, even though I already knew the answers. I was struggling to rise above despair. I was not able to portray a Christ-like attitude because I was consumed with physical pain. I slept exhausted, holding on to one truth: God loves me.
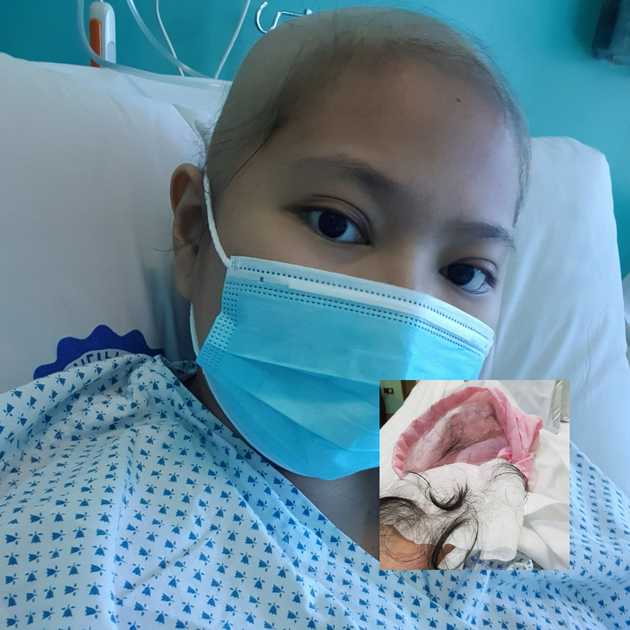
I was then informed that my WBCs are enough for me to be transferred to a regular room. On Day 15, I was out of the SCT unit. And five days later, I lost all my hair.
Finally, I was starting to lose the excess fluids and was closer to my admission weight. I pitied and was in awe of my body. The toil it went through was unworldy.
I thought I was on my way to discharge. But on Day 21, I was breathless, and I had intense pain on my left upper abdomen. I had a CT scan, which showed fluid on my right lung and micro nodules on both lower lobes. I had a chest ultrasound, which measured the fluid at 400 mL. The plan was to drain the fluid the next day through a procedure called thoracentesis.
God is truly full of compassion and mercy. When they checked the fluid right before the procedure, it was barely 30 mL. The procedure was cancelled. And on Day 24, I was able to go home.
Looking back to my month-long hospitalization, from May 9 to June 10, I see that I was never forsaken. God was with me in that hospital room, and God continues to be with me.
I am humbled by my dependence on God and others. From the beginning, my family has done everything to keep me alive. My mother and sister have always been with me. My father and brother, though are back home, have always supported me. Our extended families and friends have always been one call away. And strangers have always been there to help.
As of this writing, I’m on Day 75. Since discharge, I have weekly blood works and consultations. I am on a lot of medicines, and I have been dealing with side effects, such as graft-versus-host disease. Post transplant is another chapter of my story. There are fears of relapse, rejection, and complications. And I have to learn to rise above them. I hope to share what’s been happening, but I’m still treading unsurely. Meanwhile, let us praise God that I made it through the transplant!